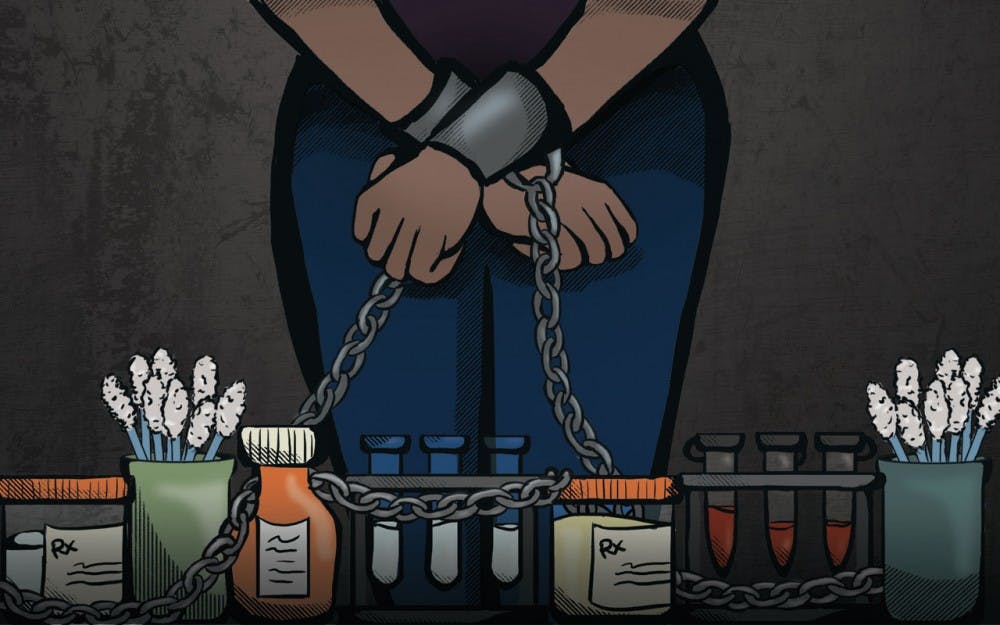
A murky legal path
E didn't know about legal options when she was diagnosed with herpes.
Skye David, an attorney for the N.C. Coalition Against Sexual Assault, said those who pursue legal action often file civil lawsuits for personal injury and negligence.
Laws address the issue differently in each state. North Carolina restricts knowingly infecting someone with an STI through its public health laws. Violating these laws could result in a misdemeanor charge and up to 2 years in prison, but punishments are rare.
HIV-positive individuals are legally required to disclose status to partners under specific circumstances. They must wear condoms unless they have been virally suppressed for at least 6 months, their partner is taking medication to prevent infection or their partner is also HIV-positive.
With other STIs, such as chlamydia and gonorrhea, health codes require individuals to refrain from having intercourse until treatment is completed and to notify recent partners.
When someone is diagnosed with syphilis or HIV, a disease intervention specialist is legally obligated to notify all partners.
Michelle Camarena, assistant director of nursing at Campus Health, said after diagnosing students, medical professionals tell students it's their legal obligation to inform their partners of their status. Then, Campus Health tells the students the clinic must report STIs to the Orange County Health Department.
Cases are easier to win if the STI is incurable, like HIV and herpes. If a partner doesn't get infected from exposure, it doesn’t always mean the perpetrator can avoid charges. In some states, HIV or another STI status can result in a harsher punishment for sexual assault.
But some individuals exposed to STIs nonconsensually may not want to take legal action.
“I don’t know if I would have even wanted or had any options to report,” E said.
Rachel Valentine, executive director of the Orange County Rape Crisis Center, said many people who come to the center do not know about STI-related laws. The center is trying to change that through its education programs.
To get the day's news and headlines in your inbox each morning, sign up for our email newsletters.
“It is often very helpful when we are talking with young people about sexual coercion and sexual assault to be able to cite that, you know, this isn’t just something that we believe is wrong or hurtful or harmful — this is actually something our state legislature has codified into law,” she said.
Informed consent
It can be difficult for people to define what they’ve experienced when they contract an STI from a partner who didn’t disclose their status, creating a barrier to reporting.
"When somebody’s consent has been violated, or they’ve been denied the opportunity to have informed consent, it takes a whole lot of empowerment for that individual to even identify what has happened to them as having been a violation,” Valentine said.
UNC’s Policy on Prohibited Discrimination, Harassment and Related Misconduct categorizes knowingly exposing a partner to an STI without the individual’s knowledge as sexual exploitation.
UNC doesn't specify when a case includes nonconsensual contraction of an STI in the annual report from the Equal Opportunity and Compliance Office.
UNC media relations manager Jeni Cook said incoming students learn about this policy through orientation and the online Haven module on sexual violence. Other campus groups also offer optional sexual education programs, including Sexual Health and Relationship Education and SAFE at UNC.
But David, a graduate of the UNC School of Law, said many students don't fully absorb what they learn in online modules.
“Even for me, it was tough to read everything and not to zone out and just click through it," she said. "People should know what is or is not a violation of your student code, local and state laws, and what your options are if something happens to you, and it’s not just a line that says ‘refer to the student handbook on this page.’”
E said she doesn't consider knowingly exposing someone to an STI as sexual assault, but someone cannot fully consent to sex without that disclosure.
“It’s obviously deception, but I actually think it definitely falls into the lines of sexual misconduct,” she said.
An individual's STI status can also be used as a tool of abuse. E’s ex-boyfriend told her that no one would accept her if she left him.
“He definitely told me your typical abuser thing — ‘No one will want you because you’re a whore, and you’ve already been infected,’” she said.
Even though E knew he had infected her, she still felt like she had somehow done something wrong.
“I was like, ‘Wow, I can’t believe I let this happen to me,’ which sounds absurd,” E said. "But that’s the sort of ideation you go through when you’re in that type of relationship.”
Rob Stephenson, director of the Center for Sexuality and Health Disparities at University of Michigan, said young people often understand what prevents STIs, but the problem lies in their ability to have a conversation with a partner.
E said she has a responsibility to tell her partners about her status, one that she takes seriously — but that didn’t change her anxiety when she first told her current boyfriend about it.
“We’re all afraid of rejection. That person might consent to having sex with you, but finding out your status might change that and change your relationship, and that’s very nerve-wracking,” E said.
Her current partner agreed to take on the risk and ended up contracting herpes himself. While E said she felt guilty, it comforted her to know they had discussed the risks.
“Because there was no dishonesty from beforehand, it was easy to tell him, ‘Okay I recognize what’s happening, go to the doctor and you won’t suffer that much,’” she said.
'Reducing the stigma'
Some experts say criminalizing STI exposure might increase the stigma around being infected.
“If you live in an environment where just having a bacterial infection is a criminal offense, or passing that onto someone else is a criminal offense, of course that’s a massive barrier to wanting to go and get tested,” Stephenson said.
Thevy Chai, a director of medical services at Campus Health, said they have made efforts in the past several years to advertise vaccines and the importance of STI testing, provide easy access to contraception and keep screening costs low.
“We’re reducing the stigma. This is common practice, this is human nature, this is sexual health,” Chai said.
E said she struggled to accept her lifelong diagnosis, but she has made peace with it.
“I come from a very conservative background where people think STDs are a punishment from God for having premarital sex,” she said. “What has helped me and what has changed my view is that I need to shift the idea of an STI as a punishment to any other kind of disease mechanism."
"We don’t blame people or get upset with them when they catch a cold.”
special.projects@dailytarheel.com