U.S. Rep. Angie Craig, D-M.N., the bill's sponsor, could not be reached for comment at the time of publication.
Diabetes and Insulin
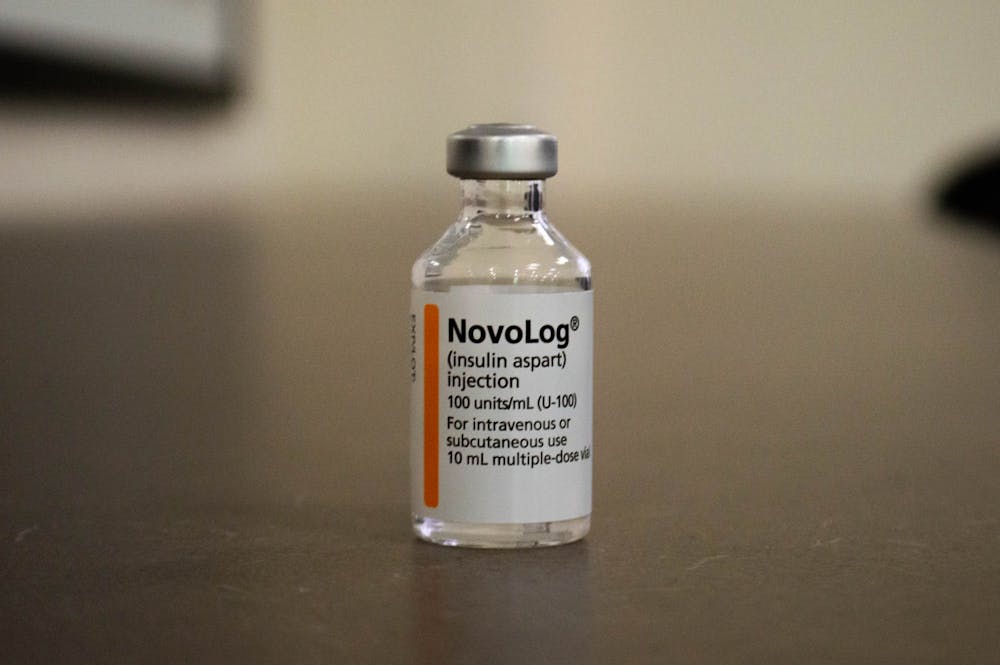
Diabetes, which has no known cure, impacts the way the body regulates blood sugar levels. Those with diabetes either fail to produce the amount of necessary insulin — a chemical that moderates blood sugar — or cannot use what they do make effectively.
“If you don't have insulin, or you don't have sufficient insulin from your own body, then you can start to feel really fatigued, you can feel sick, you can get really weak,” Rachel Selinger, a certified diabetes care and education specialist at UNC Campus Health, said.
Other long-term effects of the disease include heart disease, kidney disease and vision loss.
Diabetes comes in many forms: Type 1 diabetes, Type 2 diabetes and gestational diabetes. While treatment for each differs, insulin injections are often required to manage the disease and its health effects.
“When you have Type 1 diabetes, there's not very many other options because there's nothing that we can do to make your body make insulin,” Selinger said. “For Type 2 diabetes, there’s some things we can do to make your body more sensitive to the insulin you make, but even then, some people still need insulin.”
Diabetes in North Carolina
North Carolina currently has the 14th highest rate of diabetes in the nation, according to the Kaiser Family Foundation.
Over 1 million people have diagnosed diabetes in North Carolina, which comprises around 12.4 percent of the adult population and costs $10.6 billion in the state every year. Around 244,000 more people across the state are believed to have the disease but remain undiagnosed, according to the ADA.
“It’s pretty urgent, to say the least,” Allston said.
She also said that increased insulin prices have led those with diabetes who are also low-income to face additional challenges. Insulin prices increased 14 percent annually between 2012 and 2018, according to the American Action Forum.
To get the day's news and headlines in your inbox each morning, sign up for our email newsletters.
Though some states, including Colorado and New Mexico, have attempted to address these rising prices with copay caps that minimize costs to users who have insurance, North Carolina has not.
“While North Carolina does offer insulin coverage in state insurance plans, they only cover 700,000 people who may or may not need insulin,” Allston said. “We have a rough estimate of 1.3 million diabetics in a state with no copay caps, price caps or emergency insulin laws.”
And though the Affordable Insulin Now Act would institute a national copay cap system at $35 or less, Allston said that those who don't have insurance would see no change in prices.
“The uninsured are left out of the equation again,” she said.
Other policy options
Allston said the best policy to address rising insulin costs would be a price cap, which would limit how much insulin producers can charge for products.
She said that such a measure would ensure all people, regardless of insurance status, could afford life-saving insulin — something she argued a copay cap simply couldn’t do.
And while there is little opportunity for reform at the local level, universities like UNC have taken efforts to support diabetic students.
Campus Health Director of Pharmacy Amy Sauls said UNC's Student Blue plan has opportunities for financial aid, includes a $15 copay for a month’s supply of insulin and doesn’t require students to pay the day they pick up their medication.
“There are a lot of chronic illnesses that require medications,” Sauls said. “We try to make sure our students have access to them without having to spend all their money.”
@harrisonggummel
@DTHCityState | city@dailytarheel.com