"It angers me because of the fact that here we sit, and the people that need it the most in North Carolina can't get it," Snyder said. "But somebody who works here but lives in another state could come in and get it."
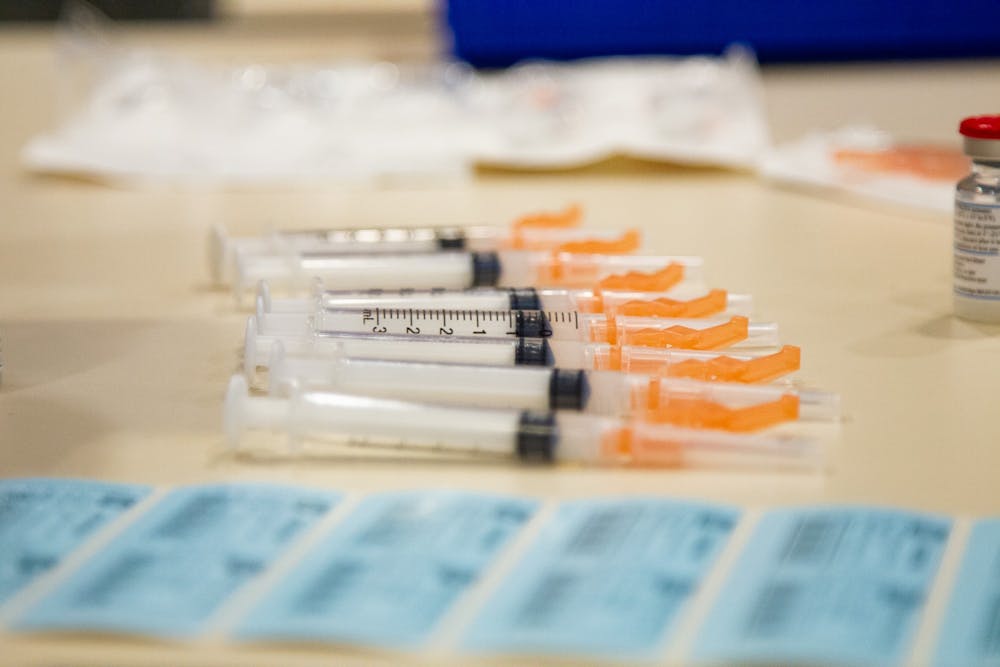
After months of checking vaccine waitlists at hospitals and pharmacies across North Carolina, Snyder said she was finally able to schedule Todd to get his first shot in late March at Walgreens.
“We are willing to drive the whole state of North Carolina to get this vaccine,” Snyder said.
Supply vs. demand
The restrictions of the phased rollout aren’t the only challenges in the distribution line. Issues from a lack of accessibility to difficulties achieving racial equity have also plagued the state’s rollout.
Mark Lyons, interim vice president of pharmacy at UNC Health, oversees the distribution of COVID-19 vaccines at 15 UNC Health entities across 12 counties in North Carolina.
Meeting the demand for vaccines has been especially challenging with a limited supply, he said.
“If supply was not an issue, there would be vaccine on every corner drugstore,” Lyons said. “And there would be vaccine at every health care system, at every health department.”
Since mid-December, UNC Health has vaccinated more than 200,000 people. But Lyons said this past week was the first time UNC Health has had enough vaccines to meet their weekly capacity of 20,000 doses.
As the number of vaccines allocated by the state starts to increase, Lyons hopes the “queuing effect,” of eligible individuals being unable to secure appointments, will lessen.
N.C. State University Professor of Biological Sciences Vicki Martin echoed this sentiment. For more than a week, Martin said she spent nearly five to six hours a day continuously refreshing clinic websites — even checking between the hours of 3-5 a.m. — and calling county health departments in an attempt to get her 87-year-old mother vaccinated.
“These websites are basically circular sites that once you get on there, you go ‘round and ‘round and ‘round, and there's really not a lot of information,” she said.
To get the day's news and headlines in your inbox each morning, sign up for our email newsletters.
Eventually, Martin, who is 66 years old and lives in Fuquay-Varina, was able to get an appointment scheduled for both her mother and herself in Harnett County. When she got the phone call from the Harnett County Health Department, she said she teared up.
But, Martin said the hoops she had to jump through to get to that point were exhausting. Both Snyder and Martin tried several times to voice their frustrations about the piecemeal vaccine rollout via phone calls and emails left with state officials, including Cooper.
“We have 100 counties in North Carolina, and there (are) no commonalities to any of this madness, (this) process on how to get scheduled for an appointment,” Martin said. “They're all doing different things and no one seems to be talking to each other.”
During the vaccine search process, Martin said she also kept thinking about elderly people who aren’t adept with technology and the internet, and would have no idea how to navigate the distribution system.
“It really is a shot in the dark,” she said. “No pun intended.”
Ethical dilemmas
Gabriel Lázaro-Muñoz is a bioethicist for the Center for Medical Ethics and Health Policy at Baylor College of Medicine. Lázaro-Muñoz said a general anxiety to move on from COVID-19 and the restrictions of a limited vaccine supply have spawned a series of moral quandaries as states fumble the rollout and the pandemic rages on.
If the overall goal is to save as many lives as possible, it is important to prioritize those who are at the highest risk of dying from COVID-19, Lázaro-Muñoz said. That means not driving across county or state lines to acquire a vaccine — doing so could, in theory, mean taking away a vaccine intended for someone else.
“If you're in a ship that's slowly sinking, you wouldn't elbow a grandma to get into a lifeboat before she does; you would help her,” he said. “And the people that are not eligible, they're basically elbowing the grandma.”
Getting the vaccine incidentally, like as a volunteer at a clinic at the end of the day, poses another ethical dilemma. The shelf life of the vaccine means there are time constraints around when it can be used, but Lázaro-Muñoz said if it comes down to a few leftover vials at the end of a day, individuals in eligible groups should still receive priority.
Ultimately, Lázaro-Muñoz said for young people and those without conditions that place them at heightened risk for COVID-19, the temptation to skip the line should be tempered with the reality that there are people who have a greater need for the vaccine.
Martin feels similarly. Despite the initial chaos and confusion of the vaccine rollout, she’s hopeful that the system will improve, especially as more and more people secure appointments.
“If we can put up a rover on Mars, we can certainly deal with handing out vaccinations within our country,” she said.
@MaydhaDevarajan
@DTHCityState | city@dailytarheel.com